Frequently Asked Questions about Cognitive Therapy
How Long Does Therapy Take?
Cognitive therapy is a short-term treatment model. Although treatment is always tailored to the individual’s unique difficulties and circumstances, the course of therapy for most disorders is 8-15 sessions. Some clients respond more quickly to treatment, while others require a longer course of therapy to attain optimal results. Booster sessions are often encouraged to prevent a relapse of symptoms and to reinforce client’s self-help skills. Clients like short-term, focused therapy to alleviate problems, which saves them time and money.
What Happens during the Course of Therapy?
First Session
The therapist’s most important job is to promote a strong working alliance with the client. This is primarily done by conveying empathy and understanding of the client’s problems. The client is helped to explore the difficult thoughts and feelings that may need to be altered.
The initial session is usually devoted to determining if cognitive therapy is the suitable treatment and identifying problem areas with accompanying goals of treatment. We also consider whether medication might be a helpful adjunct to treatment.
In the initial session we develop a list of the client’s problems and symptoms and begin to translate these into target goals. The client is given feedback on his difficulties and how cognitive therapy might be helpful.
What Happens in the Second Session?
By the end of the second session, we have begun to identify the distortions in thinking and unproductive behavior patterns that contribute to the client’s difficulties. A treatment plan that spells out the steps and techniques to help reduce symptoms and solve the client’s problems will be presented. The client should have a clear understanding of the course of therapy through a case formulation that includes:
(1) a detailed listing of the client’s problems and symptoms
(2) the relevant distortions in thinking and unproductive behavior patterns that contribute to the client’s difficulties
(3) agreed-upon realistic treatment goals
(4) a clear-cut treatment plan which spells out the steps and techniques to help solve the client’s problems and reduce symptoms.
What’s Next?
During the next several sessions, the client and therapist work in a collaborative manner to address the client’s immediate concerns and to reduce suffering. The cognitive therapist is active and directive. The client is taught a range of emotional and behavioral self-control skills. We try to provide clear rationales for treatment strategies and give the client explicit feedback about his or her problems and possible solutions. Progress toward treatment goals is measured.
Sessions typically have the following structure:
1. Client and therapist collaboratively set an agenda for the session, which involves trying to resolve a current concern.
2. The therapist facilitates problem-solving by choosing from a range of cognitive, behavioral, and experiential strategies.
3. Therapist and client review the session and consider “homework” that might be helpful.
Near the end of therapy, we help the client identify the basic attitudes and assumptions that may need to be altered to reduce future episodes of distress. We also teach specific relapse prevention techniques.
In the final stage of treatment, we help the client identify those basic beliefs and assumptions that may need to be altered to reduce future episodes of distress. We also teach specific relapse-prevention techniques.
Is Medication Used?
Treatment effectiveness for some difficulties may be enhanced with the use of medication. We will discuss the pros and cons of using medication, as well as provide information about research on the usefulness of medication with different disorders. If a client is already on medication, we will coordinate treatment with that provider. If a client is considering medication, we will refer the client to a psychopharmacologist, a specialist who can provide guidance and treatment.
How Is Progress Assessed?
Two key features of cognitive therapy are measurement and feedback. We administer mood scales and other psychological tools to measure progress objectively. We encourage ongoing feedback regarding progress and any perceived obstacles to treatment.
What is the Theory behind Cognitive Therapy?
Cognitive therapy is based on the seminal work of Drs. Beck and Ellis.
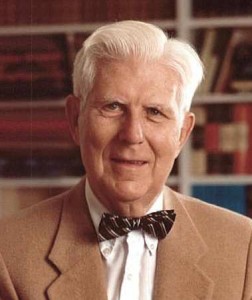
Dr. Aaron Beck
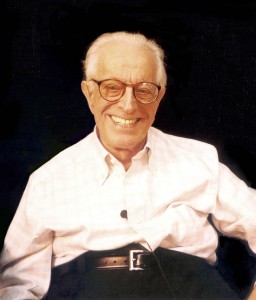
Dr. Albert Ellis
Drs. Beck and Ellis, although originally trained in psychoanalysis, developed treatment models highlighting the direct role of thinking in emotional distress. A good deal of research and clinical observation has validated the link between negative, dysfunctional thinking and human suffering.
The key finding in the cognitive model is the recognition that much of this negative thinking is distorted to increase suffering. When these twisted thinking patterns can be identified and replaced with more accurate and flexible thinking, significant improvement can occur.
The cognitive model developed by Dr. Beck and the “Rational-Emotive Therapy” model of Dr. Ellis emphasize the critical role of core beliefs. Core beliefs are basic and fundamental ways we view ourselves and the world. Individuals with harsh and rigid core beliefs are particularly vulnerable to mood or behavioral difficulties. Examples of core beliefs include: “I am worthless”, “I am incompetent”, “No one could love me”, “I must excel in my work”, “ It’s too dangerous to express my feelings”, “I must do whatever it takes to get others approval” Bringing such maladaptive beliefs out in the open and helping clients develop more compassionate and constructive frameworks promotes deeper and more durable change.
We want to express our appreciation to these pioneers of cognitive therapy, Dr. Beck and Dr. Ellis, and to those who developed newer proven treatments, such as Dr. Jeffrey Young for schema-focused therapy and Dr. Leslie Greenberg for emotion-focused therapy.